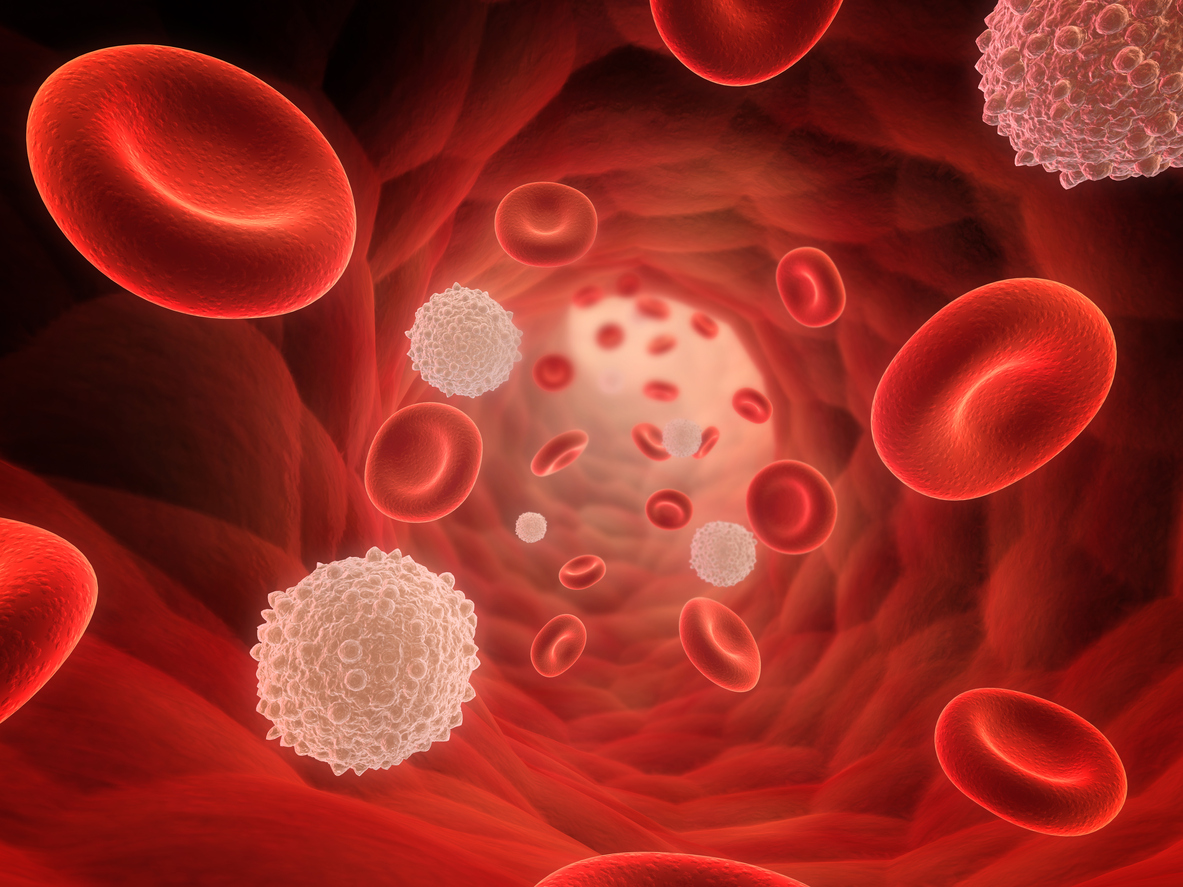
White blood cells are the defenders of our body, protecting us from germs and sickness. Imagine them as superheroes with special powers. They can move anywhere in our body to find and fight germs.
Moreover, some act like tiny vacuum cleaners, eating up and destroying germs. Others are like clever detectives, recognizing and tagging germs for destruction. What’s amazing is they have a memory – if they’ve met a germ before, they remember it and can fight it faster next time.
In simple terms, these cells are our immune system’s superheroes, always on guard to keep us well.
White Blood Cells Unveiled: Guardians of the Immune System

White blood cells, or leukocytes, are the superheroes in your bloodstream that fight off infections. When there’s an elevated number of these cells, we call it leukocytosis.
In adults, about 60 to 70 percent of white blood cells, specifically the granulocytes, are produced by the bone marrow. The lymphocytes, making up 20 to 30 percent, come from places like the thymus, spleen, and lymph nodes. Monocytes, accounting for 4 to 8 percent, are produced by organs like the spleen, liver, and lymph nodes.
Furthermore, a healthy adult usually has between 4,500 and 11,000 white blood cells per cubic millimeter of blood. These numbers can change throughout the day, with lower values when you’re at rest and higher values during exercise.
They are like little powerhouses. Also, need continuous energy production to stay alive, and their chemical processes are more complex than those of red blood cells. These cells, with a nucleus and the ability to produce RNA, can make proteins.
Now, when it comes to chronic granulomatous disease, it messes with the normal functions of neutrophils, a type of white blood cell. Most white blood cells hang out in tissues, not just in the bloodstream, doing their infection-fighting duties. They’re specialized for different tasks, and although they don’t divide in the bloodstream, some still have the ability to do so.
So, in a nutshell, white blood cells are the defenders against infections, and they’re pretty versatile in their roles.
Types of White Blood Cells
Here are some of the key types of white blood cells:
Neutrophils: These guys are like the foot soldiers of the immune system. They’re quick responders, rushing to the site of infection to engulf and destroy invaders.
Lymphocytes: There are two main types:
- T Cells: These are like the commanders, orchestrating the immune response. Some directly attack infected cells, while others help regulate the immune system.
- B Cells: These are the antibody factories. They produce proteins called antibodies that tag invaders for destruction.
Monocytes: These are like the cleanup crew. They can transform into macrophages, large cells that engulf and digest pathogens, and dead cells.
Eosinophils: Specialized in dealing with parasites and involved in allergic reactions. They release substances to destroy parasites and modulate immune responses.
Basophils: They release histamine, a chemical involved in allergic responses. Think of them as the alarm bells that signal other immune cells when something’s not right.
Natural Killer (NK) Cells: These are the assassins. They target and destroy infected or cancerous cells directly, playing a crucial role in immune surveillance.
Each type has its unique role, but they work together like a well-choreographed dance to keep the body safe. It’s a fascinating and intricate defense system!
Adaptations of Phagocytes in Immune Defense
Phagocytes, specialized white blood cells crucial for the body’s defense against infections, showcase various adaptations facilitating their efficient response to pathogens. These adaptations include:
Irregular Shape and Pseudopodia: Phagocytes boast an irregular shape with flexible pseudopodia extensions, enabling them to engulf even large or irregularly shaped pathogens.
Amoeboid Movement: Capable of amoeboid movement, it can crawl through tissues, aiding their migration towards infection sites for effective pathogen elimination.
Phagocytosis: The process where phagocytes engulf pathogens involves pseudopodia extending around the pathogen, forming a phagocytic vacuole for subsequent digestion.
Lysosomes and Reactive Oxygen Species (ROS): Moreover, it vacuoles fuse with lysosomes, containing digestive enzymes that break down engulfed pathogens. Additionally, phagocytes generate ROS, potent antimicrobial molecules contributing to pathogen destruction.
Pattern Recognition Receptors (PRRs): Expressing PRRs on their surface, phagocytes recognize specific pathogen patterns, initiating the phagocytosis process.
Toll-Like Receptors (TLRs): TLRs, a type of PRR, specifically recognize bacterial and fungal components, signaling phagocytes to activate antimicrobial mechanisms and trigger an inflammatory response.
Fc Receptors: Expressing Fc receptors, phagocytes bind to the Fc portion of antibodies. This enhances the engulfment and destruction of antibody-coated pathogens.
Plasticity and Adaptability: It exhibits adaptability in functions and metabolism in response to environmental cues and various pathogen types, allowing it to effectively combat a broad spectrum of infections.
Adaptations of Lymphocytes in the Adaptive Immune System
Lymphocytes, pivotal players in the body’s adaptive immune system, possess specialized features crucial for recognizing and eliminating specific pathogens. These adaptations include:
Antigen Recognition: Lymphocytes feature diverse surface receptors recognizing specific antigens and unique markers on pathogen surfaces.
Antibody Production: B lymphocytes produce antibodies upon encountering specific antigens, contributing to immune response amplification.
Memory Cells: Subsequent encounters lead to memory cell formation, providing long-term immunity against specific pathogens.
T Cell Receptor (TCR) Diversity: T lymphocytes express TCRs recognizing antigen fragments on cell surfaces, facilitating targeted responses.
Helper T Cells and Regulatory T Cells: Helper T cells coordinate immune responses, while regulatory T cells control and prevent autoimmune reactions.
Cytotoxic T Cells: Specialized in killing infected or cancerous cells, cytotoxic T cells release molecules to destroy target cells.
Recirculation and Tissue Homing: Lymphocytes circulate between blood and lymphatic systems, patrolling for pathogens and homing to specific tissues.
Costimulation and Activation Signals: Activation requires antigen recognition and additional costimulatory signals from antigen-presenting cells (APCs).
Immune Checkpoints: It expresses immune checkpoints, regulating immune responses to prevent damage to healthy tissues.
Exploring White Blood Cell Disorders: A Peek into Imbalances
Our body’s defense system, led by white blood cells, is quite a complex team. Let’s simplify things:
Normal Changes: Newborns start with a high white blood cell count, which gradually decreases as they grow. Lymphocyte count, however, starts low, peaks in the first four years, and then settles into an adult level. This journey mirrors the natural course of our immune development.
Leukocytosis – The Rise: When there’s an abnormal increase in white blood cell count, we call it leukocytosis. This usually happens due to more granulocytes, especially immature ones. Intense physical activity, strong emotions, pain, pregnancy, and certain diseases can trigger this. It can also be a red flag for leukemia, a blood cancer involving excessive white blood cells.
Leukopenia – The Drop: On the flip side, a decrease in white blood cell numbers is leukopenia. It can be linked to infections, medications, or conditions like chronic anemia or malnutrition.
Infections and Their Tales: Some infections tell specific stories. Viral infections often lead to lymphocytosis, an increase in small lymphocytes. Chronic infections like tuberculosis may cause mild lymphocytosis. Then there’s infectious mononucleosis, where the Epstein-Barr virus leads to atypical large lymphocytes. These special cells are part of the defense team against the virus and disappear when the battle is won.
Understanding White Blood Cell Conditions: Signs, Tests, and Care
Signs and Symptoms:
- Fever, Body Aches, and Chills: Feeling under the weather.
- Red, Swollen Wounds: Boo-boos that don’t want to heal.
- Frequent Infections: More sick days than usual.
- Persistent Cough or Breathing Issues: Not just a regular sniffle.
Normal White Blood Cell Count:
Around 4,000 to 11,000 cells per tiny drop of blood (microliter) is the usual range. You produce around 100 billion white blood cells every day – that’s your immune system in action!
Common Tests:
- Complete Blood Count (CBC): A blood test that spills the beans on your blood cell details.
- White Blood Cells Scan: This involves tagging your white blood cells, putting them back in, and then scanning to spot infections or abscesses.
Low White Blood Cell Count Causes:
- Bone Marrow Issues: Like aplastic anemia.
- Cancer Invasion: Leukemia taking over the bone marrow.
- Chemo Aftereffects: Drugs hitting hard.
- Vitamin Deficiency: Especially B12.
- HIV/AIDS: The immune system taking a hit.
High White Blood Cell Count Causes:
- Autoimmune Disorders: Think lupus or rheumatoid arthritis.
- Infections: Viral (like tuberculosis) or bacterial (sepsis).
- Leukemia or Hodgkins Disease: Cancer playing its cards.
- Allergies: Your immune system on overdrive.
Treatments:
Depends on the diagnosis and severity:
- Vitamins and Antibiotics: Boosting and fighting.
- Bone Marrow Surgery or Transplant: Serious repairs.
- Blood Transfusions: A cellular refresh.
- Stem Cell Transplants: A reboot for the immune system.
Taking Care of Your White Blood Cells:
- Hygiene Matters: Keep infections at bay.
- Vitamin Boosts: Feed your immune system.
- Address Medical Conditions: Treat issues causing white blood cell hiccups.
Your white blood cells are your body’s defenders, so treat them well!
FAQ’s
Q1: How is a white blood cell specialized to perform its function?
A1: White blood cells lack hemoglobin, have a nucleus, and are capable of motility. They defend against infection by ingesting foreign materials, destroying infectious agents, and producing antibodies.
Q2: How is plasma adapted to its function?
A2: Plasma is well adapted to transport substances as it can carry a large variety of materials, including carbon dioxide and glucose. Its solubility in water allows efficient transportation around the body.
Q3: What are the 3 ways white blood cells protect us?
A3: White blood cells protect us by producing antibodies, producing antigens, and engulfing pathogens. These defense mechanisms guard against infections and diseases.
Q4: What are Specialised white blood cells?
A4: Lymphocytes are specialized white blood cells found throughout the body. B lymphocytes (B cells) mature in the bone marrow, while T lymphocytes (T cells) mature in the thymus, playing vital roles in the immune system.
Q5: How are platelets adapted to their function?
A5: Platelets can change shape and form tentacles, helping plug broken blood vessels and prevent infections. They play a crucial role in forming scabs to aid in wound healing.
Q6: What are the 7 functions of blood?
A6: Blood serves various functions, including transporting oxygen and nutrients, forming blood clots to prevent excess bleeding, carrying cells and antibodies for fighting infections, bringing waste products to the kidneys and liver for filtration, and regulating body temperature.
Final Word
White blood cells showcase incredible adaptations that make them the superheroes of our immune system. Their ability to move freely, perform phagocytosis like tiny vacuum cleaners, recognize antigens as clever detectives, and develop a memory for faster responses is nothing short of remarkable.
In addition, these adaptations are like a well-coordinated defense strategy, ensuring our body stays protected from infections and diseases. White blood cells truly embody the resilience and efficiency of our immune system, standing as vigilant guardians of our overall health.